Better Sleep for Busy Parents: Science-Backed Solutions from Pregnancy to Postpartum
- Emmanuel Uribe
- Sep 23, 2025
- 17 min read
Sleep stands as a vital yet delicate pillar of health. Expecting and new parents face the challenges of pregnancy, late-night feedings, and work schedules, all while their bodies undergo significant physiological changes. It's precisely when sleep is most crucial that many parents find it increasingly elusive.
This article aims to maintain scientific rigor and practical applicability by examining sleep from various perspectives:
Essential sleep requirements during pregnancy and postpartum
Common sleep challenges for mothers and fathers
Nutrients and supplements for restful sleep without health risks
Behavioral and environmental strategies, including sleep hygiene, mattress choice, and noise machines
Practical tips for busy parents balancing work and childcare
The Objective
To provide parents with confidence, clarity, and practical steps for improved rest.

Sleep Needs Across Parenthood
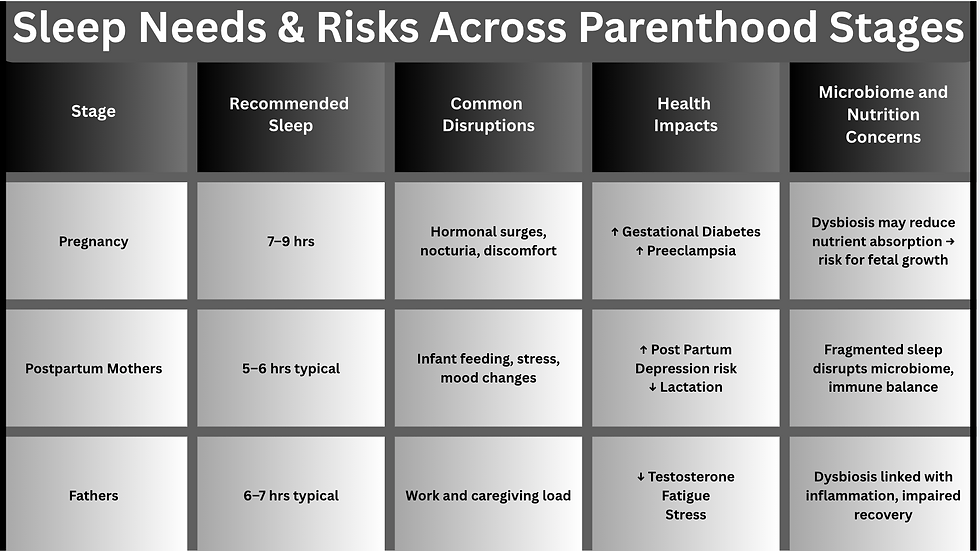
During pregnancy, postpartum, and early fatherhood, sleep requirements align with those of the general adult population—7 to 9 hours per night. However, unique physiological and environmental factors often disrupt this need.
Pregnancy
During pregnancy, hormonal changes in the body increase the requirement for restorative sleep. The American College of Obstetricians and Gynecologists (ACOG) highlights that inadequate sleep during pregnancy is associated with gestational diabetes, hypertension, prolonged labor, and an increased risk of cesarean delivery (Facco et al. 2010). As a result of these hormonal fluctuations, sleep disturbances often start in the first trimester, become more pronounced in the second trimester due to physical discomfort, and reach their peak in the third trimester with issues such as nocturia and back pain (Sedov et al. 2018).
Nocturia is waking at night to urinate, disrupting sleep and affecting quality of life. It is linked to the lower urinary tract, more common with age, and associated with sleep disorders, cardiovascular disease, and diabetes (Bosch and Weiss).
Postpartum Mothers
Following childbirth, mothers typically experience disrupted sleep, averaging 5–6 hours per night during the initial postpartum weeks (Dorheim et al. 2009). Studies indicate that sleep deprivation adversely affects mood regulation, delays postpartum recovery, and increases the risk of postpartum depression (Okun et al. 2018). Sufficient rest is crucial for successful lactation, hormonal balance, and maternal physical recovery.
Fathers
Fathers, though frequently overlooked, encounter considerable sleep disturbances. Research indicates paternal sleep is reduced by approximately one hour each night during the first six months postpartum, especially when fathers are managing caregiving responsibilities and full-time employment (Bai et al. 2016). Chronic sleep deprivation in fathers adversely affects work performance, testosterone levels, and mental health resilience (Philbrook and Teti 2016).
Gut Microbiome, Sleep Loss, and Immune Function
Emerging studies show that sleep disruption can cause gut microbiome dysbiosis, characterized by reduced microbial diversity, shifts in bacterial phyla (Firmicutes/Bacteroidetes), and overgrowth of opportunistic taxa, affecting digestion and micronutrient processing. The gut microbiota ferments dietary fiber into short-chain fatty acids (SCFAs), supports vitamin synthesis, and influences bile-acid metabolism (Knox et al.; Bäckhed et al.). Reduced diversity limits SCFA production, impairing micronutrient absorption like iron, magnesium, and B vitamins. Additionally, opportunistic overgrowth can increase intestinal permeability (“leaky gut”) symptoms, and triggering inflammation (Smith et al.; Benedict et al.).
During pregnancy, dysbiosis may affect placental function and maternal recovery. Rodent studies link sleep deprivation to reduced alpha diversity and increased Firmicutes/Bacteroidetes ratio. While human studies show limited trends (Sun et al.), one human study found greater microbiome diversity linked to better sleep, while poor sleep correlated with elevated inflammatory markers (Smith et al.).
Understanding the gut-brain-immune axis reveals how insufficient sleep can weaken immunity, delay healing, and increase infection risk. More research is needed on sleep, the microbiome, nutrient biomarkers, and fetal outcomes. For parents, inadequate sleep may affect immunity, cognitive function, cortisol levels, and relationships. Identifying sleep needs and challenges is crucial for family well-being.
Common Sleep Challenges for Moms and Dads
Even when aiming for 7 to 9 hours, both expectant and new parents often find quality sleep elusive. These disruptions arise from biological, psychological, and environmental factors that differ slightly between mothers and fathers across the prenatal, perinatal, and postnatal stages. By understanding all influences, parents can adopt coping strategies that are realistic for city life.
Biological and Psychological Factors
Prenatal Sleep Challenges
Pregnancy involves hormonal and physical challenges that disrupt rest. In the first trimester, increased progesterone causes daytime sleepiness, while nausea and frequent urination disrupt nighttime sleep (Sedov et al. 171). By the third trimester, back pain, restless legs syndrome (RLS), and gastroesophageal reflux (GERD) become major issues (Facco et al. 80). About 30% of pregnant women experience clinically significant insomnia symptoms (Mindell and Jacobson 113).
Perinatal and Postpartum Sleep Challenges
Postpartum, maternal sleep is disrupted due to hormonal changes and infant feeding demands. Variations in prolactin, oxytocin, and progesterone increase nighttime awakenings, especially with breastfeeding (Okun et al. 19). While exclusive breastfeeding is ideal for infant health, it leads to shorter sleep and frequent awakenings, particularly in the first three months (Tikotzky 73). Sleep deprivation at this stage predicts a higher risk of postpartum depression and anxiety (Okun et al. 4). In urban areas like Jersey City and NYC, noise and co-sleeping can worsen these disturbances, as mothers become very responsive to infant cues, waking at subtle sounds.
Fathers’ Sleep Challenges
Fathers, while facing fewer biological disruptions, are significantly impacted by role changes and caregiving stress. Within the first six months postpartum, they typically lose an hour of nightly sleep (Bai et al. 732), leading to chronic sleep debt (Insana and Montgomery-Downs 512). Balancing work, finances, and infant care increases sleep debt, risking burnout, lower testosterone, and reduced cognitive performance (Philbrook and Teti 591). Fathers also experience increased sleep latency due to stress or alertness when infants wake (Insana and Montgomery-Downs 145).
Shared Sleep Challenges
Sleep disturbances in parents can negatively impact immune recovery, nutrient utilization, relationship health, and cardiometabolic health, crucial for fitness goals. Circadian disruption from late-night feedings weakens rhythms, reducing slow-wave sleep and impairing immune function. Emotional stress from role adjustment increases arousal and reduces sleep efficiency. Limited exercise opportunities also diminish natural sleep drive.

Environmental Factors
Sleep disturbances are universal in prenatal and postnatal life. However, certain lifestyle barriers intensify the problem, making it vital to adopt practical coping strategies that fit real city living.
Long Commutes and Irregular Work Hours
Parents juggling work and newborn care often lose precious sleep to commutes exceeding 45 minutes each way, or to shift work that disrupts circadian rhythms (Lo et al. 691). For fathers especially, the “double shift” of long commutes plus infant duty compounds fatigue.
Coping Strategies
Micro-rest breaks: Even 20-minute daytime naps can restore alertness without causing sleep inertia.
Commute restructuring: Some parents negotiate hybrid work arrangements or staggered schedules to reclaim 30–60 minutes daily.
Sleep anchoring: Keeping a consistent “core sleep window” (e.g., dad covers 10:30p.m.–2:30 a.m., mom covers 2:30–6:30a.m.) stabilizes circadian rhythms even when wake times vary.
Urban Noise and Small-Space Living
Noise pollution from traffic, neighbors, or public transit fragments sleep (Basner and McGuire 1220). Small apartments often prolong co-sleeping arrangements, leading to parental awakenings.
Coping Strategies
Noise buffers: White noise machines, fans, or even low-level pink noise reduce arousals.
Sleep zoning: Rearranging small apartments so the sleep space is furthest from noise sources (or using blackout curtains and draft stoppers) creates a quieter microenvironment.
High Housing Density and Temperature Control
City apartments, especially older ones, can be overheated in winter or under-cooled in summer. Yet, optimal sleep typically occurs at 65–67°F (Okamoto-Mizuno and Mizuno 231). Poor thermal control worsens restlessness and sleep-disordered breathing risk.
Coping Strategies
Bed-level adjustments: Cooling mattress pads, breathable bedding, and light sleepwear can offset building-wide heating.
Portable solutions: Small portable ACs, fans, or heaters provide personal climate zones without overhauling the entire apartment system.
Digital and Social Pressures
The “always-on” NYC work culture drives late-night email and screen use, suppressing melatonin and delaying sleep onset (Harbard et al. 118).
Coping Strategies
Screen curfews: Setting “digital sunset” rules one hour before bed.
Blue light filters: If late-night work is unavoidable, blue light–blocking apps or glasses help preserve melatonin release.
Offline wind-down: Reading, gentle stretching, or mindfulness exercises reinforce nighttime cues.
Fitness and Health Trade-offs
Time scarcity often pushes exercise, meal prep, and rest down the priority list. Yet, regular activity is one of the strongest predictors of better sleep (Kredlow et al. 401).
Coping Strategies
Short-session workouts: Even 20-minute resistance or interval sessions scheduled earlier in the day improve sleep quality.
Integrated movement: Walking commutes, stroller-friendly exercise, or parent-baby fitness classes fold physical activity into childcare.
Trainer guidance: Personal trainers, especially those at Espiré Wellness, often structure programs around family schedules, helping parents avoid late-evening workouts that can delay sleep.

Sleep challenges for mothers and fathers are influenced by biological and role-specific factors, intensified by urban stressors like noise, commuting, and confined spaces. These disruptions reduce sleep duration and may worsen gut dysbiosis and nutrient absorption. Practical strategies—such as split-night schedules, noise reduction, and structured wind-down routines—help parents maintain restorative sleep, immune function, and overall health in city life.
Case 1: Maria and Daniel, Jersey City
Maria, six weeks postpartum, is breastfeeding and struggling with night sweats and frequent awakenings. Her husband Daniel has a 45-minute PATH commute into Manhattan finance, often returning home near midnight. Both report constant fatigue and irritability.
Application of Strategies
Maria invests in a cooling mattress topper and layered bedding, which helps regulate her body temperature postpartum.
The couple reorganizes their apartment to place the crib further from the street-facing window and adds a white noise machine.
Daniel negotiates a 1-day hybrid work arrangement, reclaiming almost 90 minutes of sleep per week.
They agree to a split-night schedule: Daniel covers 10 p.m.–2 a.m., Maria covers 2–6 a.m. While imperfect, this gives each a consistent 4-hour anchor block of sleep (Lo et al. 691).
Result: Within three weeks, Maria reports improved energy and reduced irritability; Daniel experiences fewer drowsy commutes and greater alertness at work.
Case 2: Priya and Alex, Manhattan
Priya, in her second trimester, is already waking frequently to use the bathroom and reports difficulty falling back asleep. Alex, a first-time father, works night shifts as a resident physician. Both live in a small one-bedroom in Upper Manhattan near a major avenue.
Application of Strategies
To offset street noise, they install blackout curtains and use pink noise apps to stabilize sound at night (Basner and McGuire 1220).
Priya begins a 20-minute stroller-walking routine after dinner (as recommended by Kredlow et al. 401), which improves sleep onset latency.
Alex uses a digital curfew and blue-light filtering glasses during his off-hours, allowing him to adjust sleep more smoothly between shifts.
Both practice “wind-down rituals” — Priya journals before bed, while Alex uses guided meditation — to reduce stress before sleep.
Result: Priya experiences fewer nights of prolonged wakefulness, while Alex notices smoother transitions between his work shifts and time at home.
These vignettes demonstrate that while urban stressors are unavoidable, targeted strategies can significantly improve parental sleep — even in high-density, high-pressure environments like Jersey City and New York City.
Nutrition and Whole-Food Strategies for Sleep
Optimizing nutrition is a critical lever for improving sleep quality in both mothers and fathers. Beyond overall caloric adequacy, specific nutrients and food timing can enhance melatonin synthesis, tryptophan transport, and microbiome health, all of which support restorative sleep.
1. Protein and Tryptophan
Tryptophan is an essential amino acid and precursor to serotonin and melatonin, key neurotransmitters regulating sleep. Protein sources high in tryptophan—such as eggs, turkey, chicken, fish, Greek yogurt, and legumes—can improve sleep onset when consumed 2–3 hours before bedtime (Markus et al. 553).
2. Carbohydrates and Tryptophan Transport
Carbohydrate intake increases insulin, which lowers competing LNAA in plasma and facilitates tryptophan transport to the brain (Wurtman et al. 749). Timing and type matter!
Complex carbohydrates (sweet potato, quinoa, oats) 1–2 hours before sleep improve tryptophan transport without causing blood sugar spikes. Avoid high-glycemic refined carbs late at night, as they may disrupt glucose regulation and sleep quality.
3. Micronutrients Supporting Sleep
Several vitamins and minerals influence sleep quality:
Magnesium: Supports GABA receptor function and muscle relaxation. Sources: spinach, pumpkin seeds, almonds.
Zinc: Linked to melatonin metabolism; found in pumpkin seeds, chickpeas, oysters.
Vitamin B6: Cofactor in serotonin/melatonin synthesis; present in bananas, chickpeas, poultry.
Together, these nutrients support both neurotransmitter production and microbiome-friendly digestion, which is particularly important for expectant parents trying to deliver optimal nutrients to the fetus (Benedict et al.; Sun et al.).
4. Safe Supplementation
For prenatal and postnatal parents:
Melatonin: Generally not recommended during pregnancy; may be considered for fathers with short-term circadian disruption, but under medical supervision.
Magnesium glycinate: Safe in recommended doses for both mothers and fathers; may aid relaxation and sleep onset.
Omega-3 (DHA/EPA): Supports maternal and fetal neurodevelopment and may improve sleep quality indirectly.
Note: Always consult a physician or dietitian before initiating supplements, particularly during pregnancy or while breastfeeding.
5. Microbiome-Supporting Foods
To mitigate sleep-disrupted gut dysbiosis eat:
Prebiotic fibers: Garlic, onion, leeks, asparagus, oats; support SCFA-producing bacteria.
Fermented foods: Yogurt, kefir, miso; enhance microbial diversity and immune signaling.
Polyphenol-rich foods: Berries, dark chocolate, green tea; support healthy bacterial phyla and reduce systemic inflammation.

Timed Eating for Sleep-Supportive Meals
Parent | Newborn Shift | Sleep Shift | Prep Start | Eat Time | Notes |
Mother | 2am-7am | 9pm-2am | 5:30 PM | 6:00 PM | Finish eating 2–3 hours before core sleep block to allow digestion; includes complex carbs + protein for melatonin transport. |
Father | 9pm-2am | 2am-7am | 10:30 PM | 11:00 PM | Later dinner ok if father’s core sleep block starts later; avoid heavy late-night meals to reduce reflux. |
Timing meals appropriately enhances tryptophan transport, supports digestion, and minimizes nighttime disruptions, which is especially important for parents in NYC/Jersey City balancing work, infant care, and split shifts.
Sleep-Supportive Meals for Busy Parents
These meals incorporate protein for tryptophan, complex carbs for transport, micronutrients, and microbiome-friendly ingredients, while remaining quick, flavorful, and suitable for NYC/Jersey City apartment living.
Vegetarian Quinoa & Lentil Buddha Bowl

Prep Tip for City Parents:
Roast sweet potatoes on a sheet pan while cooking quinoa. Assemble bowls in <20 minutes. Make extra for next-day lunch, (double ingredients).
Ingredients (serves 2)
1 cup cooked quinoa
1/2 cup cooked green lentils
1 cup roasted sweet potato cubes
1 cup fresh spinach
2 tbsp pumpkin seeds
2 tbsp miso-tahini dressing
Why it supports sleep:
Lentils provide tryptophan and B6.
Quinoa offers complex carbs for melatonin transport.
Spinach and pumpkin seeds supply magnesium and zinc.
Fermented miso dressing promotes gut health.
Vegetarian Greek Yogurt & Berry Parfait with Chia
Ingredients (serves 1)
1/2 cup Greek yogurt
1/3 cup mixed berries (blueberries, raspberries)
2 tbsp rolled oats
1 tsp chia seeds
Drizzle of honey (optional)
Prep Tip:
Can be prepared in 5 minutes and eaten cold, perfect for early mornings or post-bedtime snack.

Why it supports sleep:
Greek yogurt provides tryptophan and probiotics.
Berries supply polyphenols for microbiome support.
Chia seeds offer magnesium and fiber.
Oats at the base provide complex carbs for tryptophan transport.
Salmon, Sweet Potato, and Spinach Sheet Pan Dinner
Ingredients (serves 2)
2 wild caught salmon fillets (4–5 oz each)
1 medium sweet potato, cubed
2 cups baby spinach
1 tbsp olive oil
1 lemon juiced
Salt, pepper, and lemon zest for seasoning
Why it supports sleep:
Salmon provides tryptophan and omega-3 fatty acids for brain and fetal support.
Sweet potato delivers complex carbs.
Spinach adds magnesium.
Olive oil supports healthy digestion and microbiome function.

Prep Tip:
Toss sweet potato in olive oil and roast with salmon at 400°F for 20 minutes. Minimal cleanup, perfect for small kitchens.
Turkey & Veggie Stir-Fry with Brown Rice
Ingredients (serves 2)
1/2 lb ground turkey
2 cups mixed vegetables
1 cup cooked brown rice
1 tbsp olive oil
Soy sauce, garlic, ginger to taste
Prep Tip:
Cook in one skillet to reduce dishwashing. Use pre-cut veggies or frozen mixes to save time.
Why it supports sleep:
Turkey is high in tryptophan.
Brown rice offers slow-release carbs to support brain uptake of tryptophan.
Mixed vegetables (broccoli, carrots, bell peppers) supply micronutrients and prebiotic fiber.
Ginger or garlic enhances digestion.

Urban Family Cooking Tips
Batch prep: Roast vegetables, cook grains, or pre-portion snacks on weekends to minimize weeknight stress.
Small-space efficiency: Sheet pans, one-pot meals, and layering ingredients in bowls reduce clutter and cleanup.
Portability: Many dishes (Greek yogurt parfait, quinoa bowls) are lunchbox-friendly, suitable for parents returning to office or remote work.
Family integration: Dishes can be doubled for infant-friendly purees (e.g., steamed sweet potato, lentils, spinach) without extra effort.
Achieving restorative sleep requires attention to sleep hygiene, environmental adjustments, and monitoring tools. Even with optimal meal timing and nutrient intake, factors like noise, light, bedding, temperature, and digital distractions can affect sleep quality. We will next explore practical strategies and tools, such as temperature control, mattress selection, sleep tracking, and sound management, to ensure consistent rest for urban parents.
Sleep Hygiene, Environment, and Tracking Tools
Even with biological alignment and optimized nutrition, parents in urban settings like Jersey City and NYC face unique challenges that can disrupt sleep. Thoughtful sleep hygiene, environmental management, and selective use of tracking tools can protect restorative sleep, reduce fragmentation, and support circadian stability.
I. Environmental Factors
Noise Management
City challenges that fragment sleep include traffic, neighbors, and public transit (Basner and McGuire 1220).
Solutions:
White or pink noise machines for both parent and infant sleep areas.
Earplugs for parents when infants are co-sleeping.
Soft door/window seals to reduce urban sound penetration.
Light Exposure
City challenges include streetlights, neon signage, or electronic devices can suppress melatonin.
Blackout curtains or sleep masks.
Dim, warm lighting 30–60 minutes before sleep.
Limit screen exposure (phones, tablets, computers) before core sleep block.
Temperature and Bedding
Optimal range: 65–67°F for adults; slightly cooler for infants if safe (Okamoto-Mizuno and Mizuno 231).
Solutions:
Breathable bedding, layered sheets, or cooling mattress pads.
Portable fans or small heaters to adjust microclimate.
Lightweight, moisture-wicking sleepwear for both parents and infants.
II. Behavioral Sleep Hygiene
Consistent Sleep Schedule
Maintain core anchor sleep blocks even with staggered caregiving.
Gradual adjustments (15–30 min shifts) help align circadian rhythms.
Pre-Sleep Rituals
Wind-down routines improve sleep onset latency (Harbard et al. 118).
Examples:
Light stretching or gentle yoga.
Journaling or mindfulness meditation.
Reading physical books under dim lighting.
Limiting Stimulants and Late Eating
Avoid caffeine within 6–8 hours of core sleep.
Time meals and snacks to allow 2–3 hours for digestion before sleep.
III. Sleep Tracking Tools
Wearables and Apps
Smartwatches or ring devices track sleep duration, heart rate, and sleep stages.
Useful for parents to identify patterns, particularly during staggered shifts or disrupted nights.
White Noise and Sleep Aid Devices
App-controlled noise machines can adjust sound to match urban disruptions.
Some devices include gentle lights or temperature monitoring, reinforcing circadian cues.
Practical Consideration for Parents
Track trends rather than single-night performance.
Focus on actionable adjustments (environment, bedtime routine) rather than obsessing over metrics.
IV. City-Parent Micro Tips Integrated into Sleep Hygiene
Use portable sleep aids for temporary apartment swaps or co-sleeping rooms.
Layer sleep micro-environments: small fan + white noise + breathable bedding to optimize microclimate.
For staggered shifts, coordinate lighting and noise exposure to minimize disruption to the sleeping parent.
Employ digital reminders for wind-down rituals to reinforce habit consistency despite urban chaos.
Integrating biology, lifestyle, nutrition, and city-friendly sleep strategies allows parents to improve restorative sleep despite challenges. Sleep quality depends on circadian alignment, gut health, nutrient timing, environment, and routines, all of which support parental well-being, immune function, and infant development. When paired with practical strategies—staggered sleep blocks, batch-prepared meals, and environmental adjustments—these approaches become actionable and sustainable.
Homework Assignment: Optimizing Sleep for NYC and Jersey City Parents
Objective:
Apply the following strategies from Sections I–IV to your real-world schedule one week at a time. At the end of each week, note:
Sleep duration and quality changes
Any differences in energy, mood, or stress
What strategies were easiest/hardest to implement
Here’s to improved sleep quality over the next few months!
Step 1: Track Your Current Sleep & Meals
Week 1
Record sleep start/end times, number of awakenings, and perceived sleep quality.
Week 2
Note meal timing, content, and pre-bedtime snacks.
Step 2: Implement One Environmental Adjustment
Week 3
Add a white noise machine, use blackout curtains, or adjust bedroom temperature.
Week 4
Add another white noise machine, use blackout curtains, or adjust bedroom temperature.
Step 3: Apply One Nutrition Strategy
Week 5
Choose one sleep-supportive meal from Section III per day.
Week 6
Focus on protein + complex carbs for dinner or pre-sleep snack.
Step 4: Establish a Short Wind-Down Routine
Week 7
15–30 minutes before core sleep block: dim lights, avoid screens, perform a mindful activity like journaling, stretching, or meditation.
Week 8
Bring it all together and record your success in the comments of our blog!
Helpful Links for First-Trimester Parents
1. American College of Obstetricians and Gynecologists – Prenatal Care Overview
2. National Sleep Foundation – Sleep During Pregnancy
3. Office on Women’s Health (U.S. Department of Health & Human Services) – Pregnancy Nutrition
4. Centers for Disease Control and Prevention – Tips for Healthy Sleep During Pregnancy
5. American Pregnancy Association – First Trimester Health & Wellness
Works Cited
Bai, D., J. G. Fong, M. B. Lok, et al. “Father Involvement and Sleep in the Postpartum Period.” Journal of Family Psychology, vol. 30, no. 6, 2016, pp. 727–736.
Bäckhed, F., H. Ding, T. Wang, et al. “The gut microbiota as an environmental factor that regulates fat storage.” Proceedings of the National Academy of Sciences, vol. 101, no. 44, 2004, pp. 15718–15723.
Basner, Mathias, and Sarah McGuire. “WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Effects on Sleep.” International Journal of Environmental Research and Public Health, vol. 15, no. 3, 2018, p. 519.
Bei, B., C. Milgrom, M. Ericksen, and H. Trinder. “Subjective Perception of Sleep, but Not its Objective Quality, is Associated with Immediate Postpartum Depression Symptoms.” Sleep, vol. 33, no. 3, 2010, pp. 379–385.
Benedict, C., et al. “Gut Microbiota and Sleep–Wake Regulation.” Current Opinion in Clinical Nutrition and Metabolic Care, vol. 25, no. 3, 2022, pp. 236–242.
Bourjeily, Ghada, et al. “Sleep Disorders in Pregnancy.” Breathe, vol. 15, no. 2, 2019, pp. 122-130. PMC, https://pmc.ncbi.nlm.nih.gov/articles/PMC4989752/. PMC+2PubMed+2
Bublitz, Margaret H., Ghada Bourjeily, Christina D’Angelo, and Laura R. Stroud. “Maternal Sleep Quality and Diurnal Cortisol Regulation over Pregnancy.” Behavioral Sleep Medicine, vol. 16, no. 2, 2018, pp. 157-73. PubMed Central, https://doi.org/10.1080/15402002.2016.1210147. Sci-Hub+2PMC+2
Dorheim, S. K., K. Bondevik, A. Eberhard-Gran, and B. Bjorvatn. “Sleep and Depression in Postpartum Women: A Population-Based Study.” Sleep, vol. 32, no. 7, 2009, pp. 847–855.
Facco, F. L., E. Kramer, L. J. Ho, et al. “Sleep Disturbances in Pregnancy.” Obstetrics & Gynecology, vol. 115, no. 1, 2010, pp. 77–83.
Fernstrom, John D. “Effects of Dietary Amino Acids on Brain Neurochemistry.” The American Journal of Clinical Nutrition, vol. 77, no. 2, 2003, pp. 256–262.
Grandner, M. A. “Sleep, Health, and Society.” Sleep Medicine Clinics, vol. 12, no. 2, 2017, pp. 159–168.
Harbard, Emily, et al. “Nighttime Use of Social Media and Sleep in Adolescents.” Journal of Adolescent Health, vol. 56, no. 2, 2015, pp. 113–118.
Insana, S. P., and H. E. Montgomery-Downs. “Sleep and Sleepiness among First-Time Postpartum Parents: A Field- and Laboratory-Based Multimethod Assessment.” Developmental Psychobiology, vol. 52, no. 2, 2010, pp. 116–129.
Kredlow, M. Alexandra, et al. “The Effects of Physical Activity on Sleep: A Meta-analytic Review.” Journal of Behavioral Medicine, vol. 38, 2015, pp. 427–449.
Lo, J. C., E. Ong, K. S. Leong, et al. “Cognitive Performance, Sleepiness, and Mood in Partially Sleep Deprived Adolescents: The Need for Sleep Study.” Sleep, vol. 39, no. 3, 2016, pp. 687–698.
Markus, C. R., et al. “Effects of Tryptophan-Containing Proteins on Human Sleep.” Neuroscience & Biobehavioral Reviews, vol. 30, no. 4, 2006, pp. 553–567.
Mindell, J. A., and B. J. Jacobson. “Sleep Disturbances during Pregnancy.” Journal of Obstetric, Gynecologic, & Neonatal Nursing, vol. 29, no. 2, 2000, pp. 113–120.
Mullington, Janet M., et al. “Sleep Loss and Inflammation.” Best Practice & Research Clinical Endocrinology & Metabolism, vol. 24, no. 5, 2010, pp. 775–784.
Nakade, M., et al. “Can Breakfast Tryptophan and Vitamin B6 Intake and Morning Exposure to Sunlight Promote Melatonin Secretion in Humans?” Journal of Physiological Anthropology, vol. 33, no. 33, 2014.
Okamoto-Mizuno, Kazue, and Koh Mizuno. “Effects of Thermal Environment on Sleep and Circadian Rhythm.” Journal of Physiological Anthropology, vol. 31, no. 1, 2012, pp. 231–238.
Okun, M. L., et al. “Sleep Disturbance in Postpartum Depression: Clinical and Research Implications.” Sleep Medicine Reviews, vol. 42, 2018, pp. 1–12.
Philbrook, L. E., and D. M. Teti. “Bidirectional Associations between Sleep and Parent-Child Functioning in Infancy.” Developmental Psychobiology, vol. 58, no. 5, 2016, pp. 589–603.
Reese, A. T., et al. “Habitual Sleep Duration and the Colonic Mucosa-Associated Gut Microbiota in Humans—A Pilot Study.” Microorganisms, vol. 3, no. 3, 2020, pp. 25.
Sedov, I. D., R. L. Cameron, and L. M. Tomfohr-Madsen. “Sleep Quality during Pregnancy: A Meta-analysis.” Sleep Medicine Reviews, vol. 38, 2018, pp. 168–176.
Smith, A. L., J. E. Heiss, M. F. Harrison, et al. “Gut Microbiome Diversity is Associated with Sleep Physiology in Humans.” Journal of Sleep Research, vol. 30, no. 5, 2023, pp. e13736.
Sun, J., D. Fang, Z. Wang, and L. Liu, et al. “Sleep Deprivation Alters Gut Microbiome Diversity and Taxonomy: A Systematic Review and Meta-Analysis of Human and Rodent Studies.” Journal of Sleep Research, 2025.
Tikotzky, L. “Postpartum Maternal Sleep, Maternal Depressive Symptoms and Self-perceived Mother–Infant Emotional Relationship.” Behavioral Sleep Medicine, vol. 9, no. 2, 2011, pp. 73–88.
Wang, X.-J., et al. “Mental Health, Sleep Quality, and Hormonal Circadian Rhythms among Pregnant Women.” BMC Pregnancy and Childbirth, vol. 23, 2023, article 801, https://doi.org/10.1186/s12884-023-05801-4
Wurtman, Richard J., et al. “Carbohydrates and Brain Serotonin.” Science, vol. 210, no. 4475, 1980, pp. 749–752.
Yu, X., et al. “Maternal Sleep Deprivation in Late Pregnancy Alters Offspring Gut Microbiota and Induces Neuroinflammation.” Frontiers in Immunology, vol. 13, 2022, pp. 842721.




Comments